The Rise of Autonomous Robotic Surgery: How Close Are We?
In the annals of medical history, few innovations have sparked as much excitement—or debate—as the advent of robotic surgery. From the first FDA-approved robotic system, the da Vinci Surgical System, introduced in 2000, to today’s increasingly sophisticated machines, robotic-assisted surgery has transformed how we approach complex procedures. These systems, guided by human surgeons, have delivered unprecedented precision, reduced recovery times, and minimized invasiveness. But now, a new frontier beckons: autonomous robotic surgery, where machines could potentially operate with little to no human intervention. How close are we to this reality, and what does it mean for the future of medicine?
The Evolution of Robotic Surgery
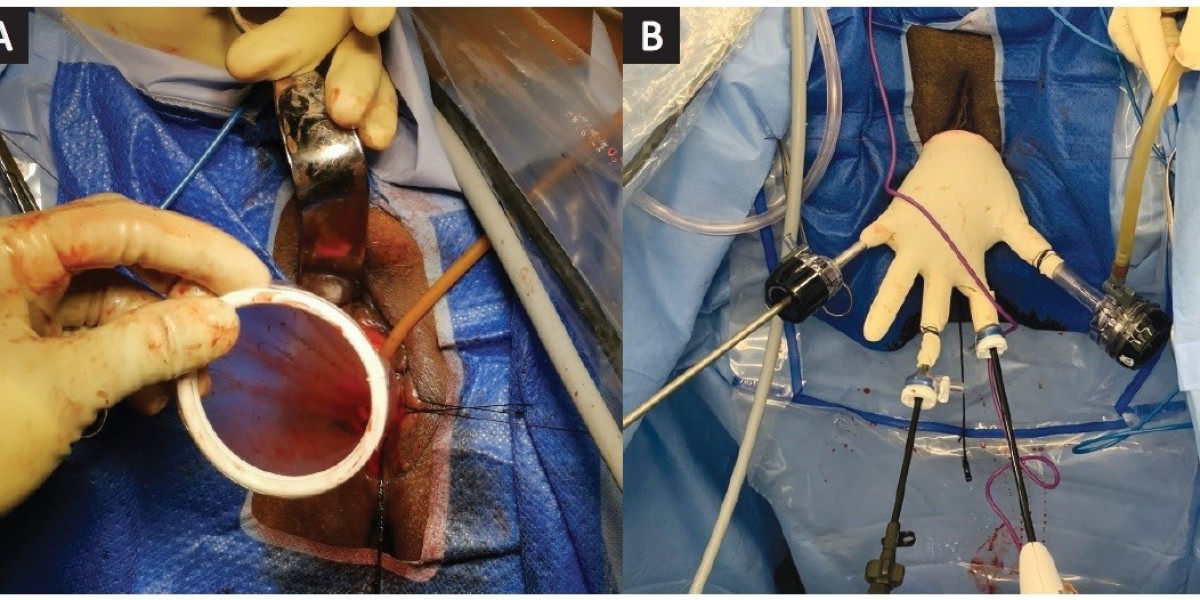
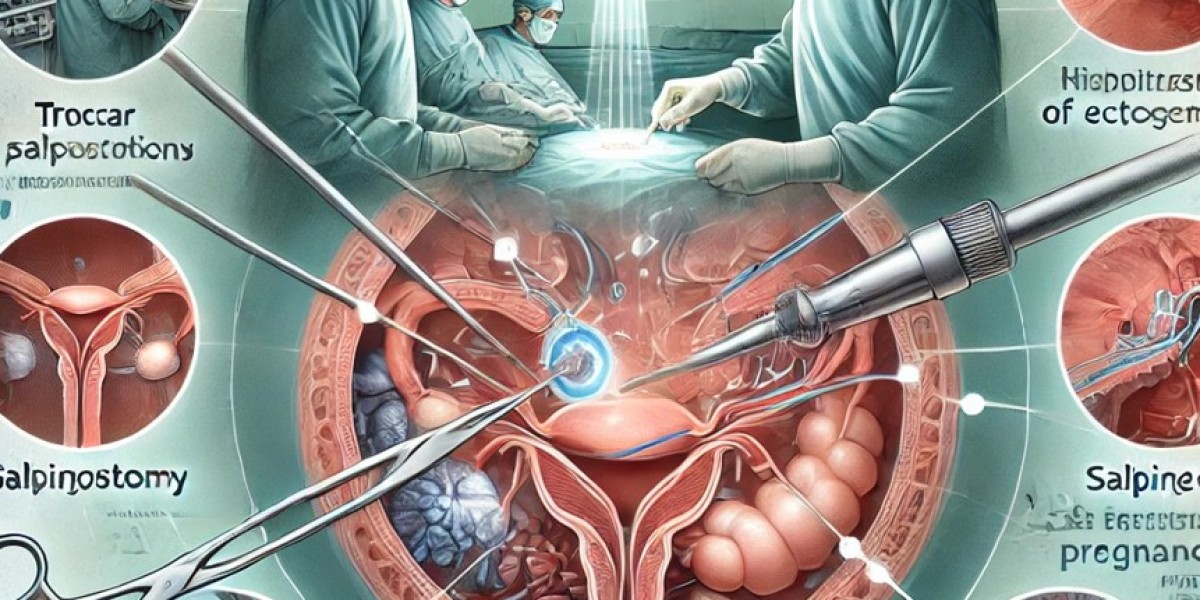
Robotic surgery began as a tool to amplify human capability. Systems like da Vinci allow surgeons to perform intricate operations through tiny incisions, using high-definition 3D cameras and robotic arms that mimic the dexterity of the human hand—but with greater steadiness and range of motion. Procedures such as prostatectomies, hysterectomies, and cardiac surgeries have seen remarkable improvements in outcomes, with patients benefiting from less blood loss, lower infection rates, and faster healing.
Yet, these systems remain entirely dependent on human oversight. Surgeons control every movement, relying on their expertise to interpret data and make real-time decisions. Autonomy, in this context, refers to a machine’s ability to perform tasks—or even entire procedures—independently, guided by artificial intelligence (AI), machine learning, and advanced sensors. The dream is a system that can execute surgeries with the precision of a robot and the judgment of a seasoned surgeon. But bridging that gap is no small feat.
Current Advances in Autonomy
The journey toward autonomous robotic surgery has already begun, albeit in small, controlled steps. In 2016, the Smart Tissue Autonomous Robot (STAR), developed by researchers at Johns Hopkins University and Children’s National Health System, made headlines when it successfully performed a soft-tissue surgery on a pig. STAR used advanced imaging, force sensors, and AI algorithms to stitch tissue with greater accuracy than human surgeons or traditional robotic systems. While human oversight was still present, this marked a proof of concept: machines could handle delicate, unpredictable biological environments.
More recently, companies like Intuitive Surgical (makers of da Vinci) and Medtronic have been integrating AI into their platforms. These advancements allow robots to assist with tasks like suturing, adjusting incisions based on tissue tension, or predicting complications by analyzing real-time data. In orthopedic surgery, systems like Mako robotic arms autonomously guide bone cuts during knee replacements, though surgeons still dictate the overall plan.
The rise of AI models capable of processing vast datasets—think of systems like those developed by xAI—has further accelerated progress. These models can analyze millions of surgical videos, patient outcomes, and anatomical variations to “learn” optimal techniques. Imagine a robot that has internalized the expertise of thousands of surgeons worldwide, adapting its approach to each patient’s unique physiology.
How Close Are We?
Despite these leaps, fully autonomous robotic surgery remains a distant goal. Current systems excel at repetitive, predictable tasks, but surgery is rarely so straightforward. Human bodies are messy—tissues shift, bleeding occurs, and anomalies abound. The best AI today can assist, but it lacks the contextual reasoning and adaptability of a human surgeon. For instance, if a patient’s artery ruptures unexpectedly, a human can improvise based on intuition and experience—something AI struggles to replicate.
Experts estimate that we’re still 10 to 20 years away from a robot performing a full, unsupervised procedure like an appendectomy or heart bypass. Dr. Peter Kim, one of STAR’s developers, has noted that autonomy will likely emerge incrementally. “We’ll see robots taking over specific subtasks—suturing, tissue dissection—before they handle entire operations,” he said in a recent interview. Regulatory hurdles also loom large. The FDA and other bodies demand rigorous testing to ensure safety, and any autonomous system would need to prove it can match or exceed human performance across thousands of cases.
The Promise and Perils
The potential benefits of autonomous robotic surgery are staggering. In regions with shortages of skilled surgeons, robots could democratize access to high-quality care. They could operate 24/7 without fatigue, reducing wait times and human error. Precision could reach new heights, with AI tailoring every cut to a patient’s anatomy. For example, a robot analyzing preoperative scans and intraoperative data might detect a tumor’s exact boundaries better than the human eye.
Yet, the risks are equally profound. Malfunctions, hacking, or algorithmic biases could lead to catastrophic failures. Who bears responsibility if an autonomous robot errs—the manufacturer, the hospital, or the AI itself? Ethical questions also arise: Can a machine truly replace the human touch, the empathy that reassures a patient before going under the knife? And what happens to the surgical profession—will it evolve into a supervisory role, or diminish altogether?
The Road Ahead
As of February 22, 2025, the rise of autonomous robotic surgery is a story of tantalizing progress tempered by formidable challenges. Research continues apace, with institutions like MIT, Stanford, and companies like Verb Surgical (a Google-Johnson & Johnson venture) pushing the boundaries of AI-driven robotics. Clinical trials are expanding, and hybrid systems—where robots and humans collaborate seamlessly—are becoming the norm.
In the near term, expect more “smart assistance” in operating rooms: robots that suggest optimal incision points, warn of risks, or take over routine tasks under human guidance. Full autonomy, however, will require breakthroughs in AI reasoning, sensor technology, and trust—both from regulators and patients.
Conclusion
The rise of autonomous robotic surgery is not a question of “if” but “when.” We stand at the cusp of a revolution that could redefine medicine, blending the cold precision of machines with the warm ingenuity of human oversight. How close are we? Close enough to glimpse the future, but far enough that the operating room remains, for now, a human domain. As technology races forward, one thing is certain: the scalpel’s next wielder may not need a heartbeat—just a brilliant algorithm.