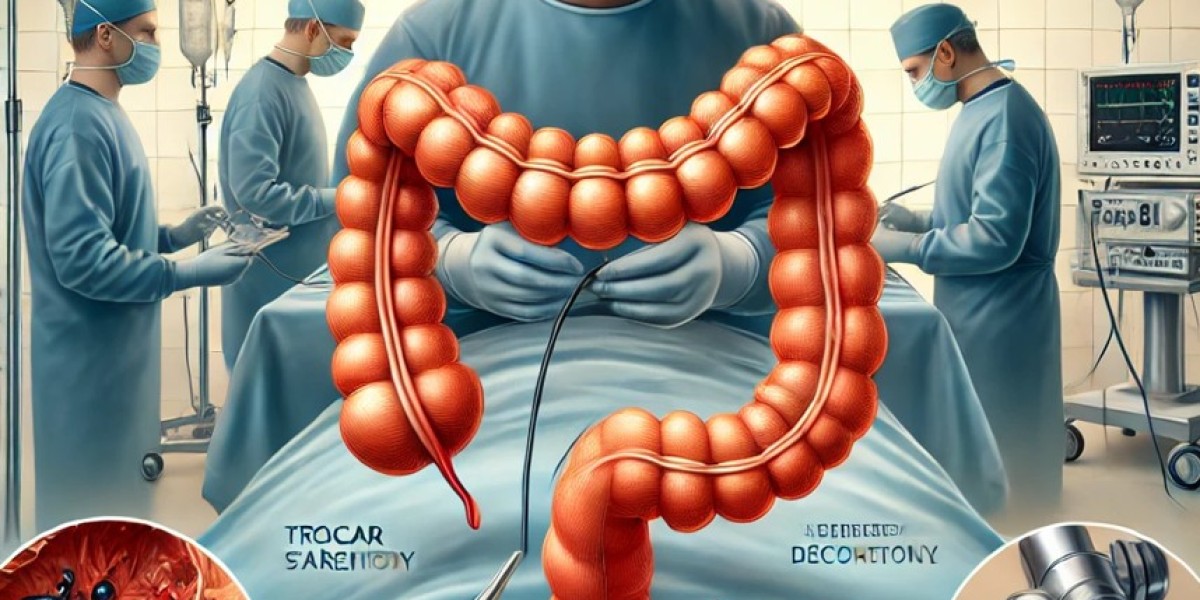
Laparoscopic Surgery for Colorectal Disorders: Benefits and Outcomes
Introduction
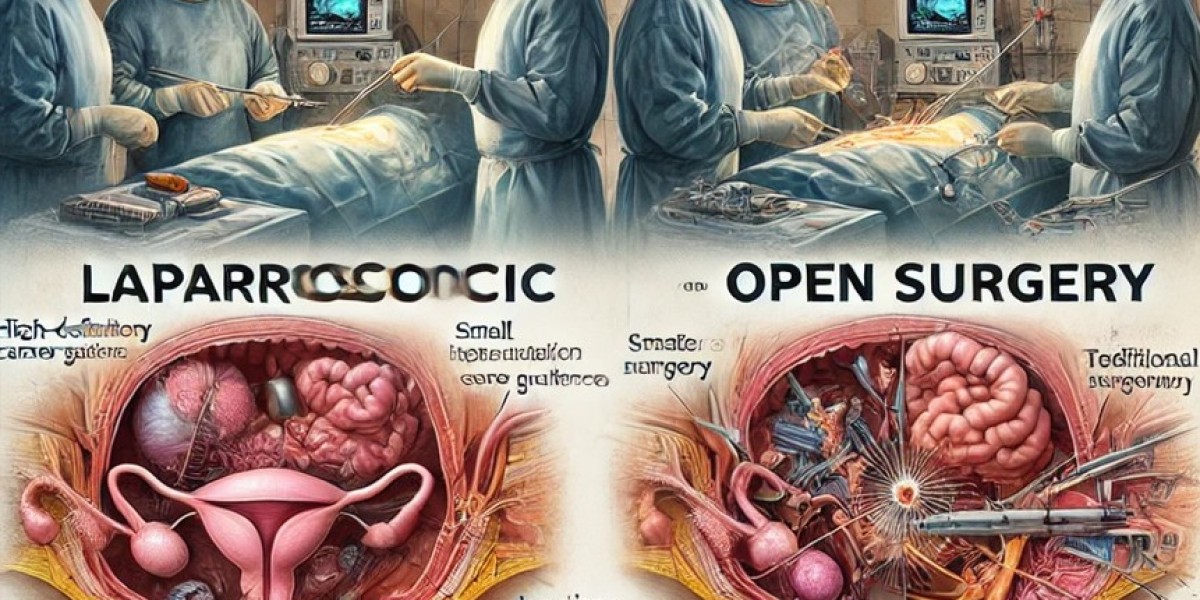
Colorectal disorders, including colorectal cancer, diverticular disease, inflammatory bowel disease (IBD), and rectal prolapse, often require surgical intervention. Laparoscopic surgery has emerged as a minimally invasive alternative to traditional open colorectal surgery, offering faster recovery, reduced postoperative complications, and better cosmetic outcomes. This article explores the role of laparoscopic surgery in managing colorectal disorders, its advantages, and patient outcomes.
Indications for Laparoscopic Colorectal Surgery
Laparoscopic techniques are widely used for the treatment of various colorectal conditions, including:
Colorectal Cancer – Partial or total colectomy for malignant tumors.
Diverticular Disease – Removal of affected segments in complicated diverticulitis.
Ulcerative Colitis and Crohn’s Disease – Proctocolectomy or segmental resections.
Rectal Prolapse – Laparoscopic rectopexy to restore rectal positioning.
Colonic Polyps – Removal of large, non-resectable polyps via laparoscopic-assisted colectomy.
Laparoscopic Surgical Techniques for Colorectal Disorders
The choice of procedure depends on the specific condition and the extent of the disease. The most common laparoscopic techniques include:
1. Laparoscopic Colectomy
Removal of a segment of the colon affected by cancer, diverticulitis, or IBD.
Performed using small incisions and precision instrumentation.
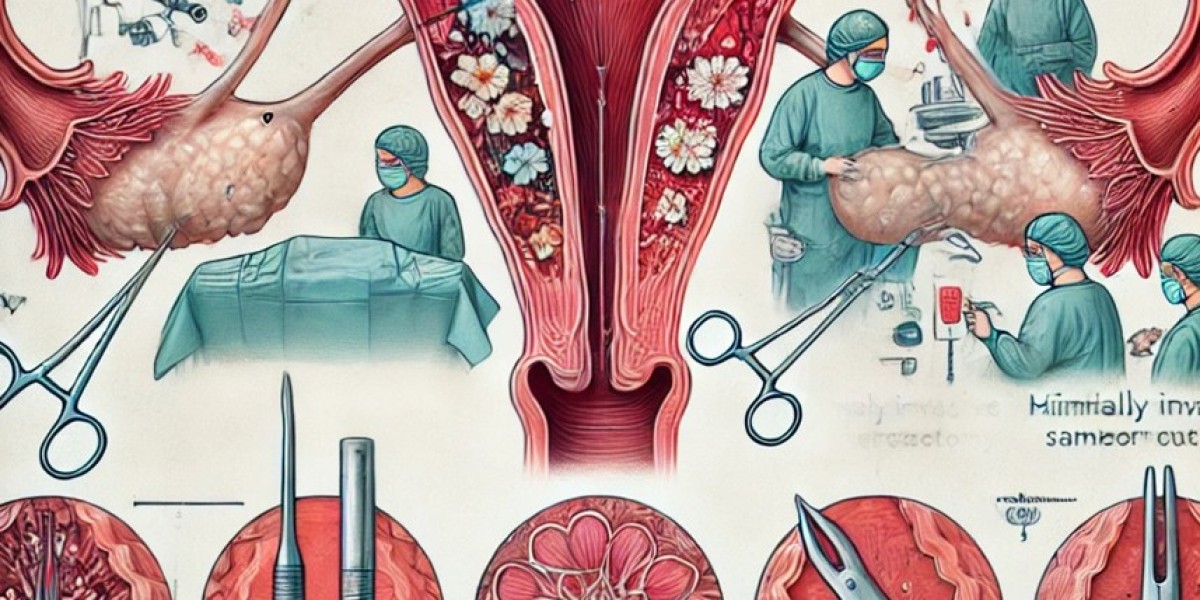
2. Laparoscopic Low Anterior Resection (LAR)
Used for rectal cancer and lower rectal diseases.
Preserves sphincter function and minimizes the need for a permanent colostomy.
3. Laparoscopic Abdominoperineal Resection (APR)
Required for low rectal tumors or cases where sphincter preservation is not possible.
Involves removal of the anus, rectum, and part of the sigmoid colon.
4. Laparoscopic Total Proctocolectomy
Indicated for ulcerative colitis or familial adenomatous polyposis (FAP).
May include an ileal pouch-anal anastomosis (IPAA) to restore bowel continuity.
5. Laparoscopic Rectopexy
Performed for rectal prolapse, securing the rectum back into place.
Benefits of Laparoscopic Colorectal Surgery
Compared to open surgery, laparoscopic colorectal procedures offer significant advantages:
1. Faster Recovery and Shorter Hospital Stay
Patients typically recover within 2-3 weeks, compared to 6-8 weeks with open surgery.
Reduced hospital stay results in lower healthcare costs.
2. Reduced Postoperative Pain and Blood Loss
Smaller incisions lead to less pain and quicker mobilization.
Minimized blood loss, reducing the need for transfusions.
3. Lower Risk of Surgical Site Infections (SSI)
Laparoscopic techniques reduce exposure of abdominal contents, lowering infection risk.
Lower incidence of incisional hernias compared to open surgery.
4. Improved Cosmetic and Functional Outcomes
Smaller scars contribute to better cosmetic results.
Preservation of bowel function and quicker return to normal activities.
5. Better Oncological Outcomes in Cancer Surgery
High-definition laparoscopy allows for precise tumor excision and lymph node dissection.
Comparable long-term survival rates to open surgery with lower morbidity.
Challenges and Limitations of Laparoscopic Colorectal Surgery
Despite its benefits, laparoscopic surgery presents some challenges:
Steeper learning curve requiring expertise in colorectal laparoscopy.
Longer operating time compared to open surgery.
Limited use in emergency cases (e.g., bowel perforation, severe bleeding).
Conversion to open surgery in cases of extensive adhesions or difficult dissection.
Recent Advancements in Laparoscopic Colorectal Surgery
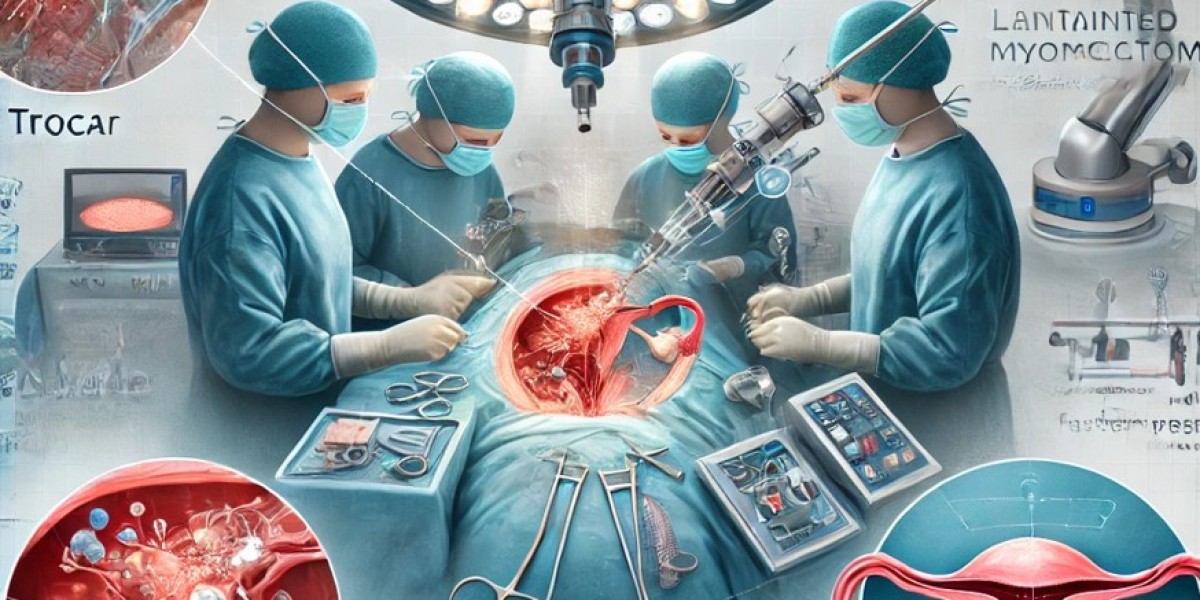
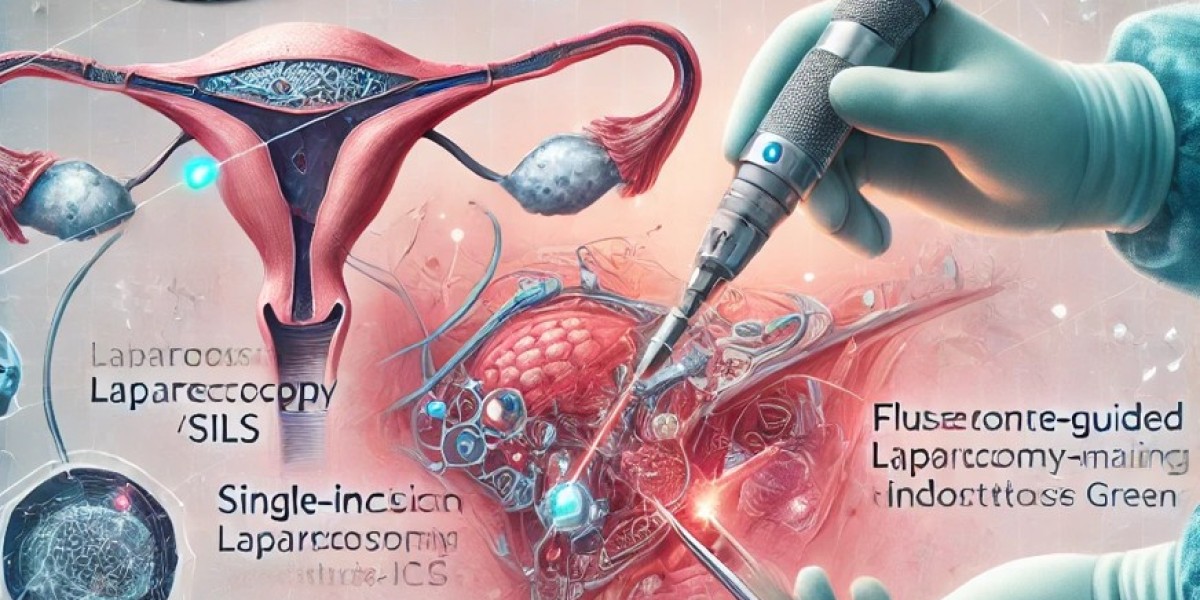
Robotic-Assisted Colorectal Surgery – Enhances precision and dexterity, particularly for rectal cancer.
Fluorescence-Guided Imaging – Improves vascular visualization and anastomotic integrity.
Single-Incision Laparoscopic Surgery (SILS) – Further reduces scarring and postoperative pain.
AI-Driven Surgical Planning – Uses machine learning for preoperative decision-making.
Postoperative Care and Recovery
Early ambulation and diet advancement to promote bowel function.
Pain management with multimodal analgesia, minimizing opioid use.
Regular follow-up for cancer patients to monitor recurrence risk.
Pelvic floor rehabilitation for rectal procedures to restore continence.
Conclusion
Laparoscopic surgery has become the gold standard for colorectal disorders, providing faster recovery, reduced pain, and lower complication rates compared to traditional open surgery. With ongoing advancements in robotics, imaging, and AI-assisted surgery, laparoscopy continues to revolutionize colorectal treatment, offering better patient outcomes and improved surgical efficiency.
For more updates on minimally invasive colorectal surgery, stay connected with the World Association of Laparoscopic Surgeons (WALS).