Cholecystectomy, particularly laparoscopic cholecystectomy, is one of the most commonly performed surgical procedures worldwide. Despite advancements in minimally invasive techniques, complications such as bile duct injury (BDI) remain a significant concern. Indocyanine Green (ICG) fluorescence imaging has emerged as a valuable tool to enhance intraoperative visualization, improve anatomical identification, and reduce the risk of complications.
The Eighth World Congress (February 21–22, 2025) emphasizes cutting-edge laparoscopic and robotic surgery, with live demonstrations and discussions on multi-specialty advancements. Dr. Goyal’s talk likely aligns with WALS’s mission—championed by Dr. R. K. Mishra—to push minimally invasive boundaries. It may also build on contemporary trials (e.g., OPRA, STAR-TREC), offering a surgeon’s practical perspective on implementing organ preservation globally.




This is a resection of segment 2 and 3 of the liver, located to the left of the falciform ligament. The tumor is in segment 2, close to where the left hepatic vein enters the inferior vena cava.
The liver is mobilized by cutting the falciform ligament and the left lobe’s connection to the diaphragm. The portal vein and hepatic artery are identified and the left branch of the portal vein is exposed.
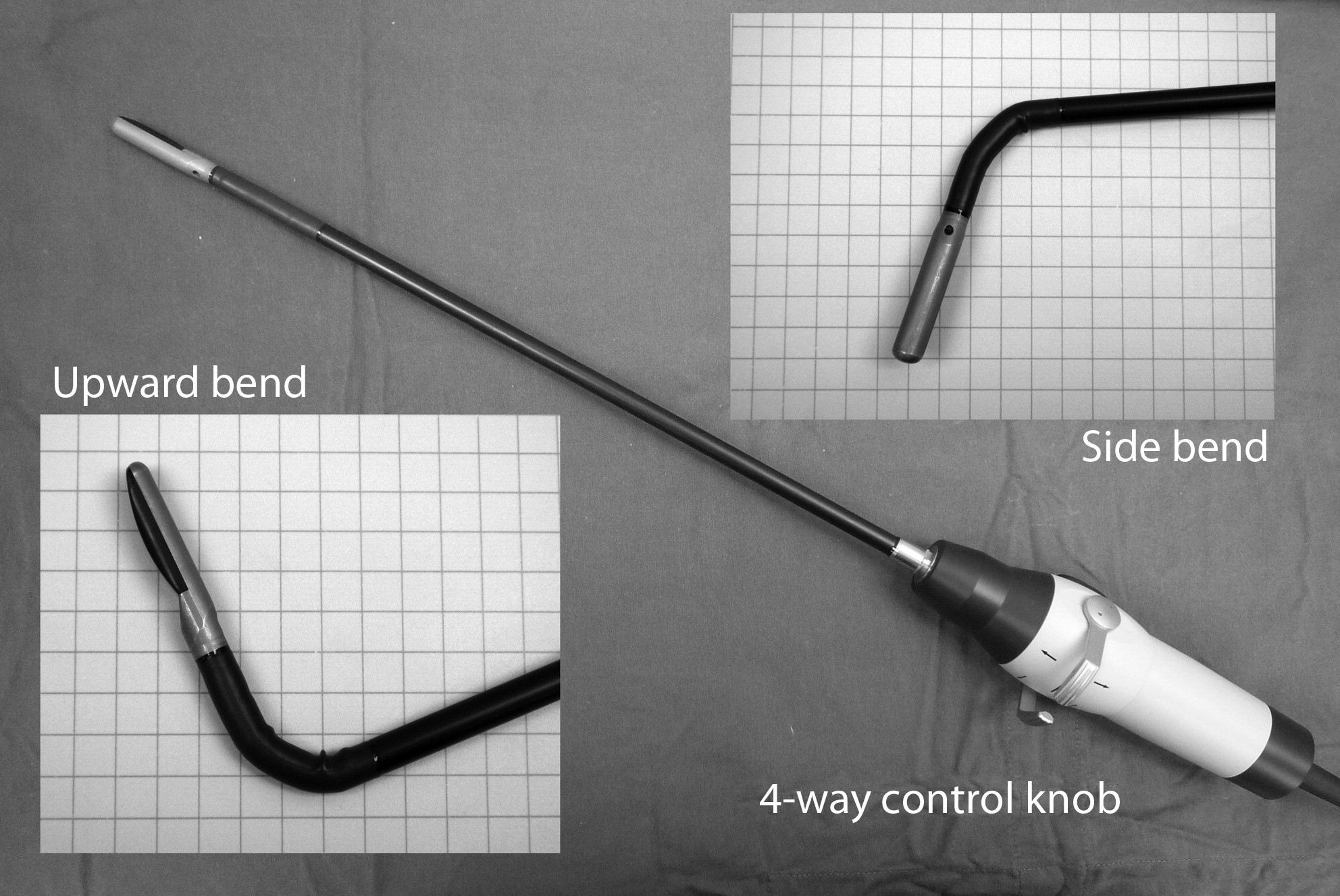
The liver capsule is cut open before an endoscopic ultrasound probe is used to locate the tumor and map the blood vessels around it. The probe is removed and the ligament is dissected up to the inferior vena cava.

Many reports have provided evidence to support the effective use of diagnostic laparoscopy and laparoscopic ultrasonography (LUS) to determine if patients with upper abdominal malignant diseases are operable so that unnecessary laparotomy can be avoided. LUS is less frequently applied to patients with pelvic malignancies and this is probably related to the technical difficulties.