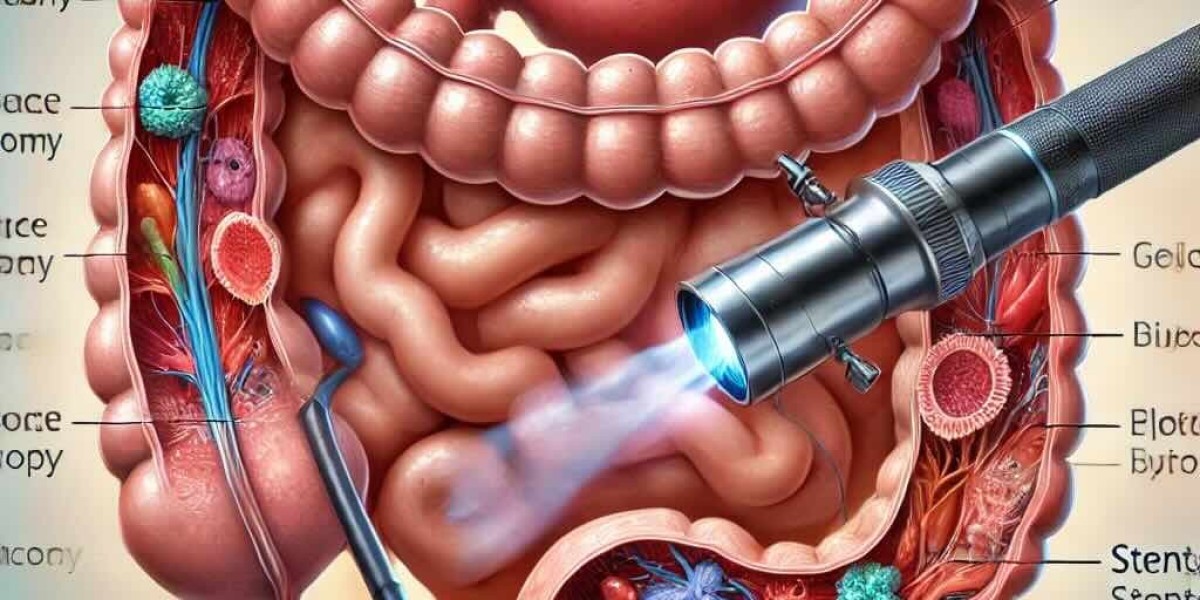
Gastrointestinal (GI) endoscopy has revolutionized the practice of surgery by providing direct visualization, diagnostic accuracy, and therapeutic interventions without the need for invasive procedures. Both upper GI endoscopy (esophagogastroduodenoscopy - EGD) and lower GI endoscopy (colonoscopy and sigmoidoscopy) play a critical role in the diagnosis, management, and postoperative surveillance of various surgical conditions.
Role of Upper GI Endoscopy (EGD) in Surgical Practice
1. Diagnosis and Preoperative Assessment
• Evaluation of Dysphagia: Identifies esophageal strictures, tumors, achalasia, and other motility disorders.
• Gastroesophageal Reflux Disease (GERD): Confirms the presence of esophagitis, Barrett’s esophagus, or strictures before fundoplication or anti-reflux surgery.
• Peptic Ulcer Disease (PUD): Detects ulcers, assesses their severity, and determines the need for surgical intervention.
• Helicobacter pylori Testing: Helps in medical management before surgical options are considered.
• Gastric and Esophageal Tumors: Preoperative biopsy and staging of malignancies guide surgical planning.
2. Therapeutic Applications in Surgery
• Endoscopic Hemostasis: For bleeding peptic ulcers, esophageal varices, and gastric vascular malformations using coagulation, banding, or sclerotherapy.
• Foreign Body Removal: Essential in cases of accidental ingestion or food bolus impaction in the esophagus.
• Esophageal Dilatation and Stenting: Used for benign and malignant strictures, reducing the need for open surgery.
• Endoscopic Mucosal Resection (EMR) & Endoscopic Submucosal Dissection (ESD): Minimally invasive resection of early GI tumors, reducing the need for radical surgery.
• Percutaneous Endoscopic Gastrostomy (PEG): Facilitates enteral feeding in patients unable to swallow postoperatively.
3. Postoperative Surveillance
• Assessment of Anastomotic Integrity: Detects leaks or strictures after procedures like esophagectomy, gastrectomy, and bariatric surgery.
• Surveillance for Recurrence: Regular monitoring in patients with a history of gastric cancer or Barrett’s esophagus.
Role of Lower GI Endoscopy (Colonoscopy & Sigmoidoscopy) in Surgical Practice
1. Diagnostic Applications
• Colorectal Cancer Screening: Essential for early detection and biopsy of polyps or suspicious lesions.
• Inflammatory Bowel Disease (IBD): Helps in diagnosing Crohn’s disease and ulcerative colitis, guiding medical or surgical treatment.
• Diverticular Disease: Evaluates diverticulosis and potential complications like diverticulitis or strictures before surgery.
• Lower GI Bleeding: Identifies and treats sources such as angiodysplasia, polyps, or rectal varices.
2. Therapeutic Applications
• Polypectomy and Mucosal Resection: Reduces the risk of colorectal cancer and eliminates the need for extensive surgical resection in early lesions.
• Endoscopic Hemostasis: Controls bleeding diverticula, angiodysplasia, or post-polypectomy hemorrhage.
• Colonic Stenting: Used in malignant obstructions to delay or avoid emergency surgery.
• Dilation of Colonic Strictures: Prevents colostomy or major resection in benign strictures.
3. Postoperative Surveillance
• Follow-up after Colorectal Surgery: Ensures anastomotic integrity and early recurrence detection.
• Surveillance in IBD Patients: Monitors for dysplasia or complications after subtotal colectomy or segmental resection.
Conclusion
Upper and lower GI endoscopy have become indispensable tools in modern surgical practice, offering early diagnosis, minimally invasive treatment, and postoperative surveillance. Their integration into surgical workflows has reduced morbidity, improved patient outcomes, and minimized the need for extensive surgical interventions. As endoscopic technologies continue to evolve, their role in surgery will further expand, enhancing patient care and broadening the scope of minimally invasive therapies.