Laparoscopic Management of Gastroesophageal Reflux Disease (GERD)
Introduction
Gastroesophageal reflux disease (GERD) is a chronic condition in which stomach acid refluxes into the esophagus, causing heartburn, regurgitation, and esophageal irritation. While lifestyle modifications and medications are first-line treatments, surgical intervention becomes necessary in patients with severe, refractory, or complicated GERD. Laparoscopic fundoplication is the gold standard for the surgical management of GERD, offering long-term symptom relief and preventing complications.
Indications for Laparoscopic Surgery in GERD
Laparoscopic surgery is recommended for GERD patients who have:
Chronic symptoms unresponsive to proton pump inhibitors (PPIs).
Severe regurgitation or aspiration-related complications.
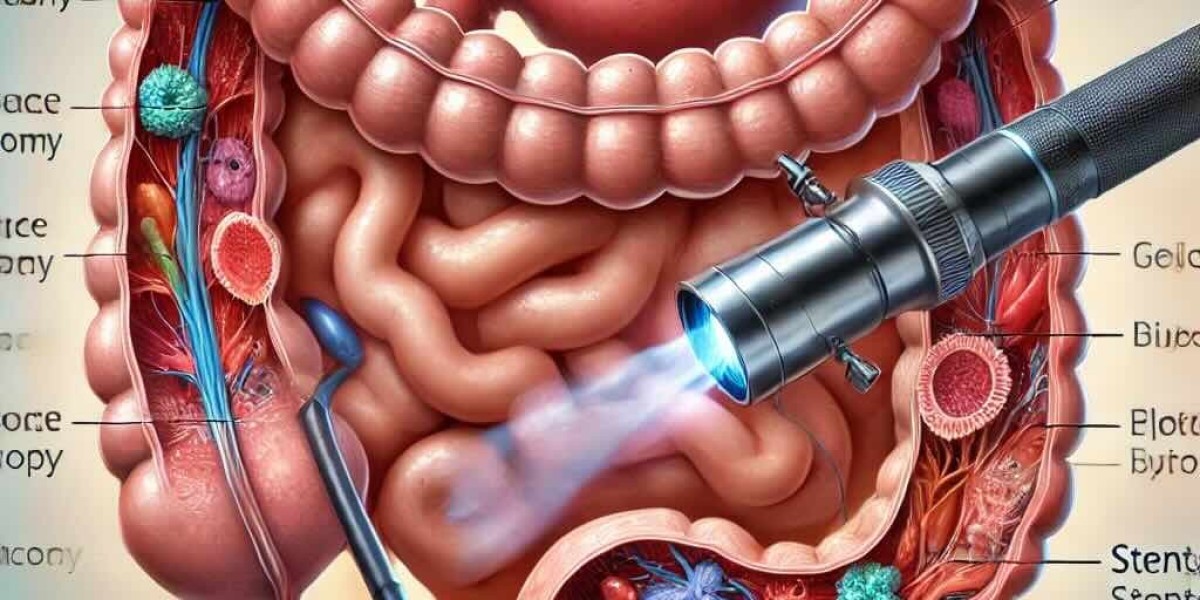
Esophagitis or Barrett’s esophagus confirmed on endoscopy.
Hiatal hernia contributing to reflux.
Young patients seeking an alternative to lifelong medication.
Respiratory symptoms like chronic cough or aspiration pneumonia.
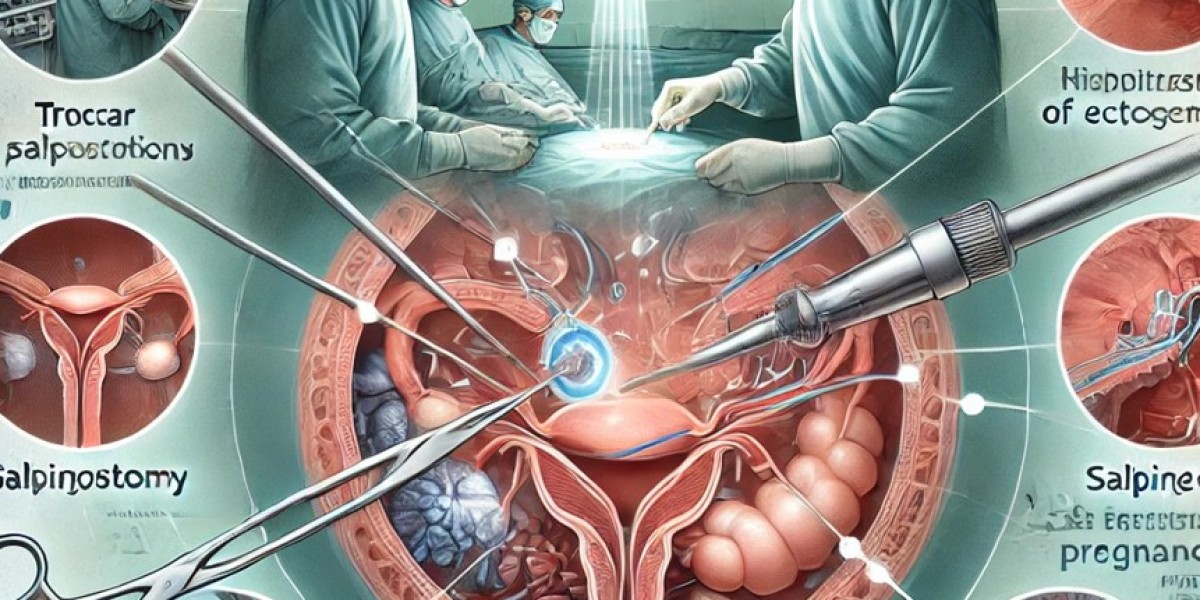
Laparoscopic Surgical Techniques for GERD
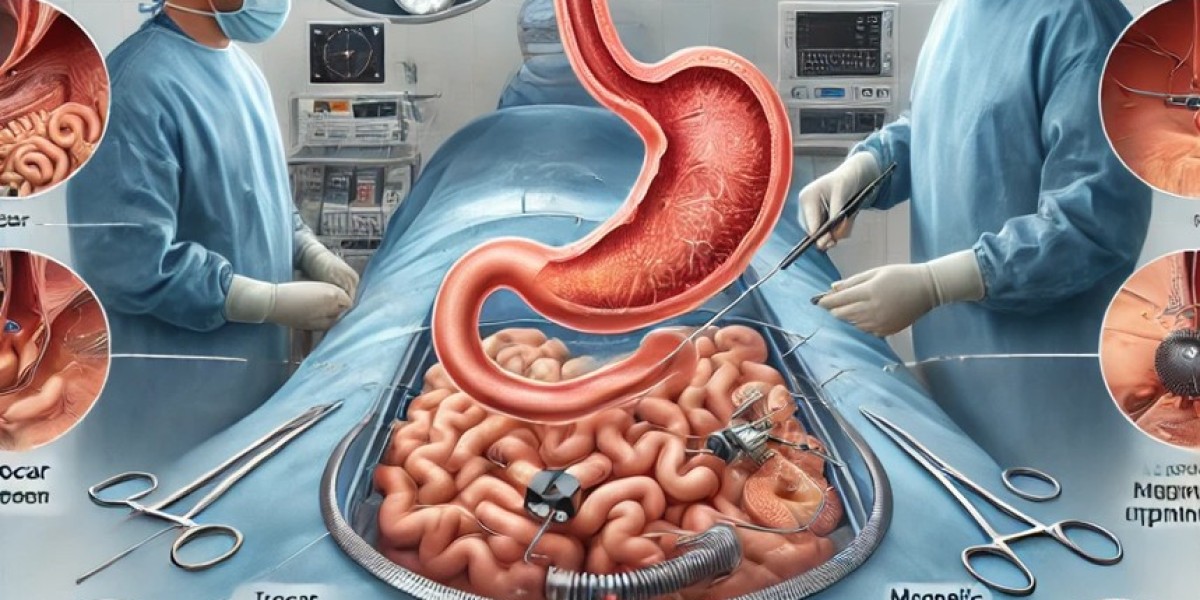
The most commonly performed laparoscopic procedures for GERD include Nissen fundoplication, Toupet fundoplication, and LINX reflux management.
1. Laparoscopic Nissen Fundoplication (360° Wrap)
The fundus of the stomach is wrapped completely (360°) around the lower esophagus to strengthen the lower esophageal sphincter (LES).
Effective for severe GERD and large hiatal hernias.
Provides excellent long-term symptom control, but may cause dysphagia in some patients.
2. Laparoscopic Toupet Fundoplication (270° Partial Wrap)
The fundus is wrapped 270° posteriorly, preserving some physiological reflux.
Ideal for patients with weakened esophageal motility.
Reduces the risk of postoperative dysphagia compared to Nissen fundoplication.
3. Laparoscopic LINX Procedure (Magnetic Sphincter Augmentation)
A magnetic ring (LINX device) is placed around the LES to reinforce its function.
Allows for physiologic swallowing while preventing acid reflux.
Minimally invasive alternative with reversible implantation.
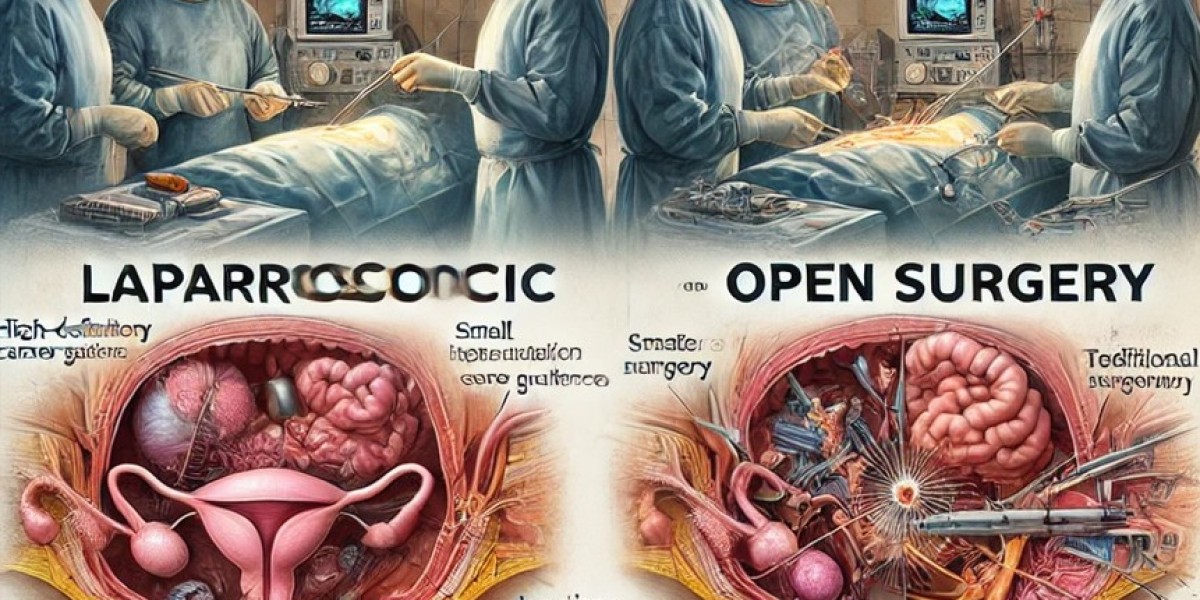
Advantages of Laparoscopic Surgery Over Open Surgery
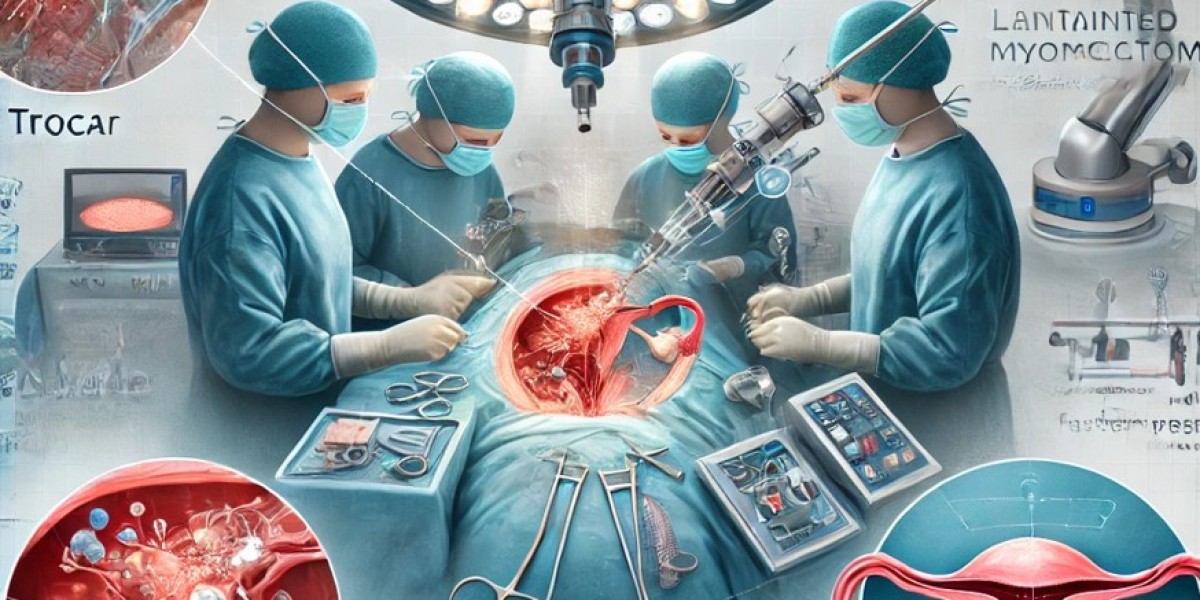
Laparoscopic techniques have revolutionized GERD treatment, offering significant advantages over traditional open surgery:
Minimally invasive approach with smaller incisions.
Reduced postoperative pain and faster recovery.
Lower risk of surgical site infections.
Shorter hospital stay, often discharged within 24-48 hours.
Faster return to daily activities.
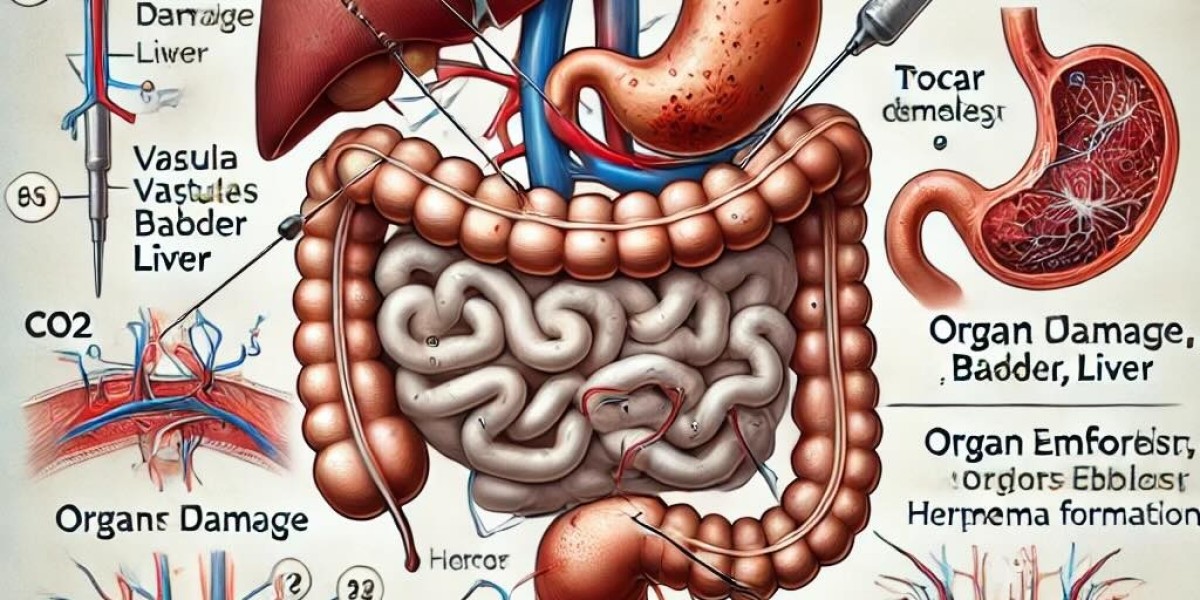
Potential Complications and Risk Factors
While laparoscopic GERD surgery is generally safe, some risks include:
Gas bloat syndrome (inability to burp or vomit after fundoplication).
Dysphagia, especially after Nissen fundoplication.
Recurrence of GERD if the wrap loosens or a hiatal hernia recurs.
Injury to the vagus nerve, affecting gastric emptying.
Rare complications like pneumothorax or esophageal perforation.
Recent Advancements in Laparoscopic GERD Surgery
Robotic-Assisted Fundoplication: Enhances precision and surgical control.
AI-Integrated Preoperative Planning: Uses machine learning for surgical decision-making.
Endoluminal Fundoplication: Performed through the mouth, eliminating external incisions.
Magnetic LES Augmentation (LINX Technology): Offers a reversible and adjustable GERD solution.
Postoperative Care and Recovery
Dietary modifications (soft food for 1-2 weeks, gradual reintroduction of solids).
Avoid carbonated drinks to prevent bloating.
Gradual return to normal activities within 7-10 days.
Routine follow-ups to monitor symptom resolution and esophageal function.
Conclusion
Laparoscopic management of GERD has transformed surgical treatment options, offering effective, long-term relief with minimal complications. With continuous advancements in robotic surgery, endoscopic techniques, and AI-driven preoperative planning, GERD surgery continues to evolve, providing better patient outcomes and faster recovery. For patients with severe or refractory GERD, laparoscopic surgery remains the gold standard for durable symptom control.
For more updates on laparoscopic advancements in GERD treatment, stay connected with the World Association of Laparoscopic Surgeons (WALS).