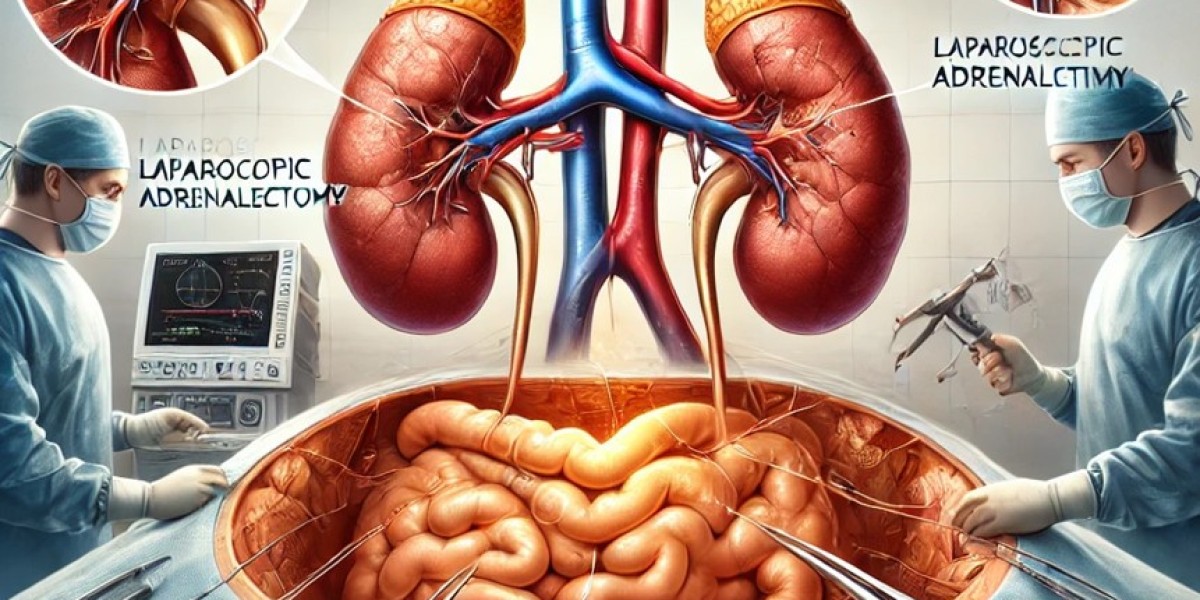
Laparoscopic Adrenalectomy: A Minimally Invasive Approach to Adrenal Tumors
Introduction
Laparoscopic adrenalectomy has become the gold standard for the surgical removal of adrenal tumors, offering a minimally invasive alternative to traditional open surgery. Adrenal tumors, whether benign, functional, or malignant, can lead to significant health complications due to hormonal imbalances or mass effects. With advancements in laparoscopic techniques, adrenalectomy has evolved into a safe, effective, and patient-friendly procedure that minimizes surgical trauma and improves recovery.
Indications for Laparoscopic Adrenalectomy
Laparoscopic adrenalectomy is indicated for patients with:
Functioning adrenal tumors (hormone-secreting tumors) such as:
Pheochromocytomas (catecholamine-secreting tumors causing hypertension).
Aldosterone-producing adenomas (Conn’s syndrome leading to hyperaldosteronism).
Cortisol-producing adenomas (Cushing’s syndrome leading to excess cortisol production).
Non-functioning adrenal tumors larger than 4-6 cm, with suspicion of malignancy.
Adrenal metastases in select cases.
Bilateral adrenal tumors in genetic syndromes such as Multiple Endocrine Neoplasia (MEN).
Surgical Technique: Laparoscopic Adrenalectomy
Laparoscopic adrenalectomy is performed using a transperitoneal or retroperitoneal approach, depending on tumor location, surgeon preference, and patient anatomy.
1. Patient Positioning and Trocar Placement
Lateral decubitus position with slight flexion to enhance exposure.
Trocar placement: Typically three to four ports (5-12mm) depending on approach.
CO₂ insufflation to create a working space.
2. Identification and Dissection of the Adrenal Gland
The peritoneum is incised, and the adrenal gland is carefully mobilized.
Major vascular structures (adrenal vein, renal vein, and inferior vena cava) are identified.
Energy devices (harmonic scalpel, Ligasure) are used for precise dissection and hemostasis.
3. Vascular Control and Adrenal Gland Removal
The adrenal vein is clipped and divided, preventing excessive bleeding.
The adrenal gland is carefully dissected and placed in an endoscopic retrieval bag.
Specimen extraction through the largest port site, minimizing tissue disruption.
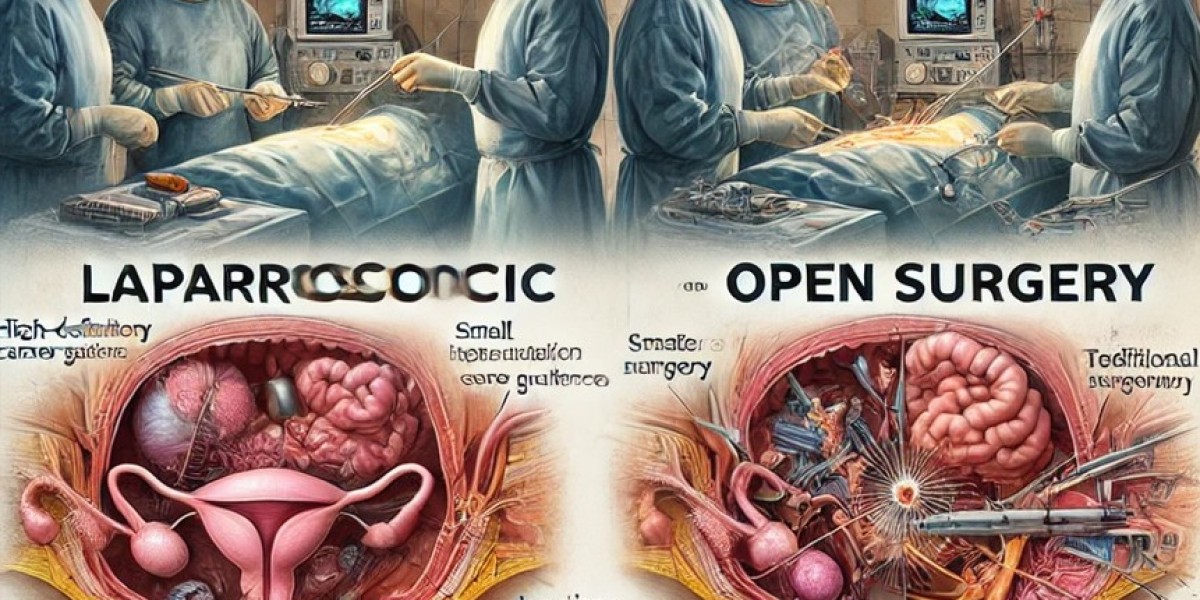
Advantages of Laparoscopic Adrenalectomy Over Open Surgery
Compared to traditional open adrenalectomy, laparoscopic surgery offers multiple benefits:
1. Minimally Invasive with Faster Recovery
Smaller incisions result in less pain and quicker healing.
Patients typically go home within 24-48 hours.
Faster return to normal activities within 1-2 weeks.
2. Reduced Blood Loss and Lower Complication Rates
Precision dissection and energy devices minimize intraoperative bleeding.
Lower incidence of surgical site infections and hernias compared to open surgery.
3. Better Cosmetic Outcomes
Smaller scars compared to a large flank or midline incision in open surgery.
4. Improved Visualization and Surgical Precision
High-definition cameras enhance anatomical visualization.
Easier identification of critical structures, reducing the risk of injury.
Challenges and Limitations of Laparoscopic Adrenalectomy
Despite its benefits, laparoscopic adrenalectomy presents certain challenges:
Difficult dissection in large adrenal tumors (>6 cm), requiring careful handling.
Risk of vascular injury due to proximity to the renal vein and inferior vena cava.
Longer operative time in complex cases compared to open surgery.
Conversion to open surgery may be required in cases of severe adhesions or uncontrolled bleeding.
Comparison: Laparoscopic vs. Open Adrenalectomy
| Feature | Laparoscopic Adrenalectomy | Open Adrenalectomy |
|---|---|---|
| Incision Size | Small (5-10mm) | Large (10-15cm) |
| Hospital Stay | 1-2 days | 5-7 days |
| Recovery Time | 1-2 weeks | 4-6 weeks |
| Postoperative Pain | Minimal | Moderate to severe |
| Blood Loss | Lower | Higher |
| Infection Risk | Lower | Higher |
| Scarring | Minimal | Prominent |
| Complication Rate | Lower | Higher |
Recent Advancements in Laparoscopic Adrenalectomy
Robotic-Assisted Adrenalectomy – Enhances dexterity, especially for complex and large adrenal tumors.
Fluorescence-Guided Imaging – Improves vascular visualization and tumor delineation.
Single-Incision Laparoscopic Adrenalectomy (SILS) – Further reduces scarring and operative trauma.
AI-Integrated Surgical Planning – Uses machine learning for personalized surgical strategies.
Postoperative Care and Follow-Up
Patients are advised to resume light activities within a few days.
Blood pressure and hormone levels are monitored for residual disease control.
Endocrinology consultation is required for patients with functional tumors.
Regular follow-up imaging may be needed for adrenal tumor recurrence monitoring.
Conclusion
Laparoscopic adrenalectomy has revolutionized adrenal tumor management, offering a safe, effective, and minimally invasive approach with faster recovery and fewer complications. With ongoing advancements in robotic surgery, AI-driven planning, and fluorescence-guided techniques, laparoscopic adrenalectomy continues to improve patient outcomes. For patients with benign or functional adrenal tumors, this approach remains the preferred surgical technique.
For the latest updates in laparoscopic endocrine surgery, stay connected with the World Association of Laparoscopic Surgeons (WALS).