The Role of Laparoscopy in the Management of Ovarian Cysts
Introduction
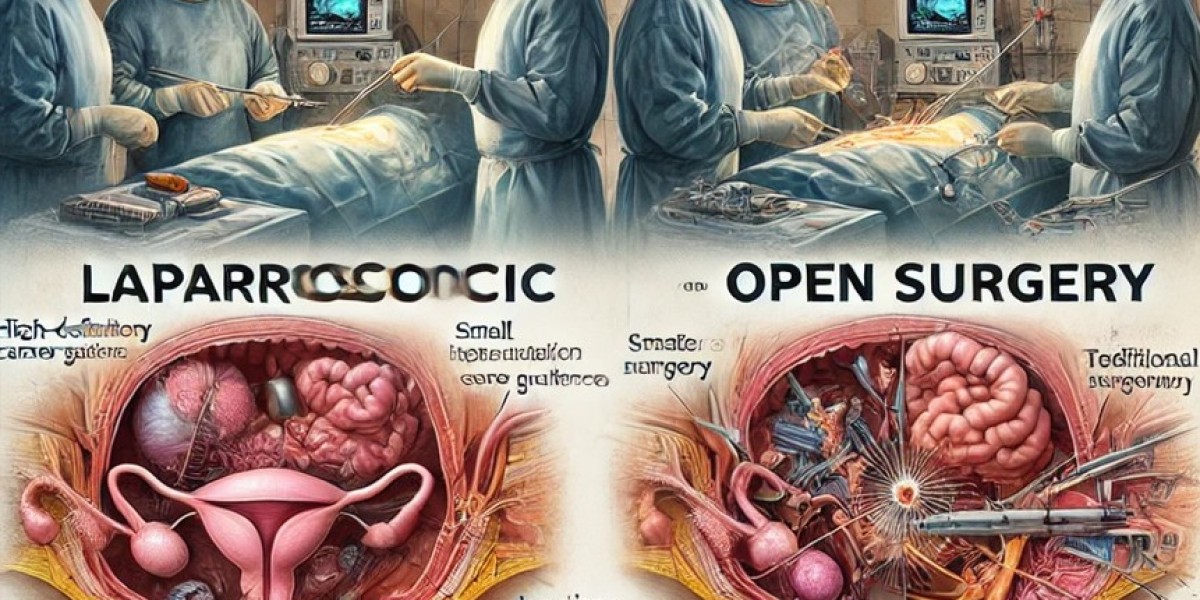
Ovarian cysts are fluid-filled sacs that develop on or within the ovary and are a common gynecological condition. While most ovarian cysts are benign and asymptomatic, some may cause pain, menstrual irregularities, or complications such as rupture or torsion. Laparoscopic surgery has become the gold standard for the management of ovarian cysts due to its minimally invasive nature, faster recovery, and lower risk of complications compared to open surgery.
Indications for Laparoscopic Management
Laparoscopic surgery is indicated in cases of:
Symptomatic ovarian cysts causing pain, bloating, or menstrual irregularities.
Persistent or enlarging cysts despite conservative management.
Complex or hemorrhagic cysts identified on ultrasound.
Ovarian torsion, requiring immediate intervention.
Suspicion of malignancy, necessitating histopathological examination.
Endometriotic cysts (chocolate cysts) affecting fertility or causing severe pelvic pain.
Polycystic ovary syndrome (PCOS) in cases requiring ovarian drilling.
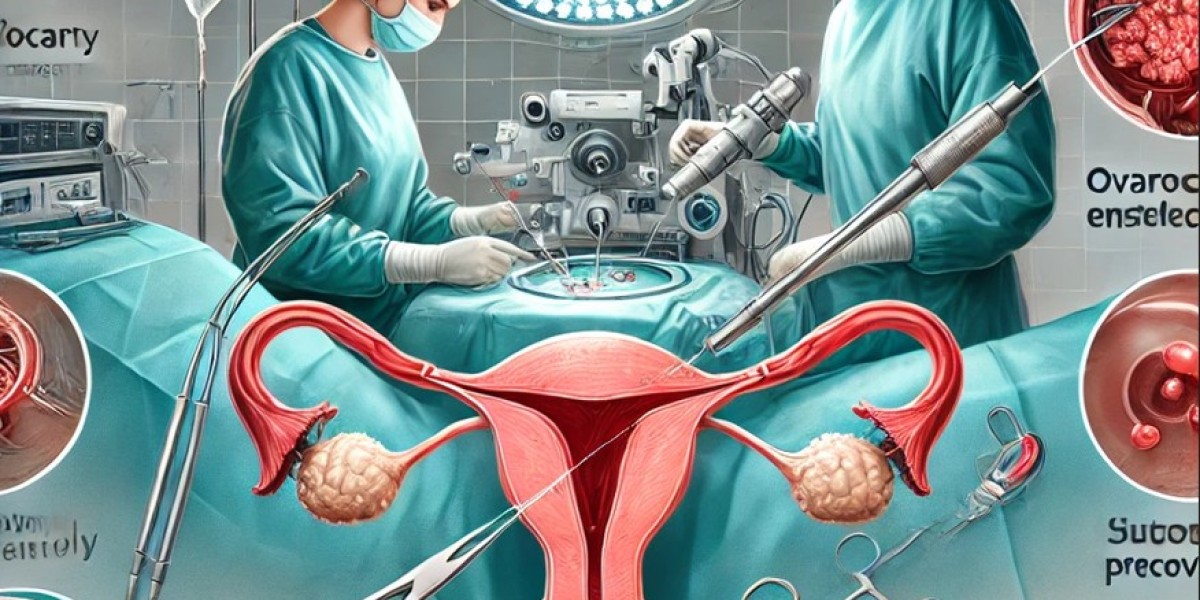
Surgical Techniques in Laparoscopic Ovarian Cystectomy
The procedure is performed under general anesthesia and involves the following steps:
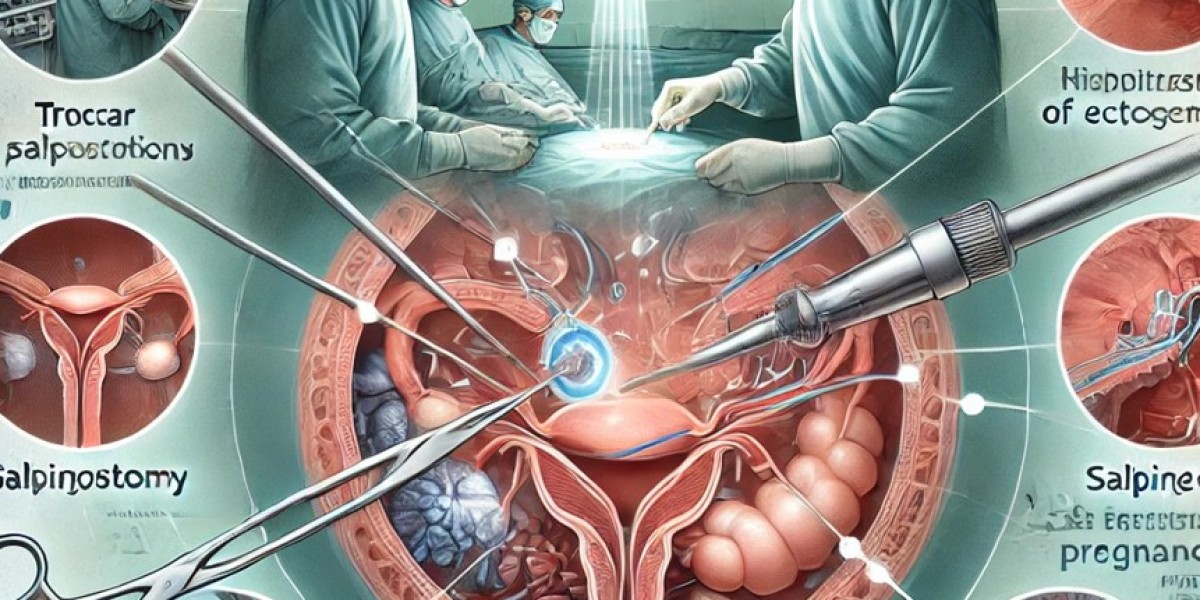
1. Patient Positioning and Trocar Placement
The patient is placed in a lithotomy position with Trendelenburg tilt to optimize visualization.
Pneumoperitoneum (CO₂ insufflation) is established.
Trocar placement: Typically one umbilical 10mm port for the laparoscope and two or three 5mm accessory ports for instruments.
2. Identification and Dissection of the Cyst
The affected ovary is stabilized using atraumatic graspers.
The ovarian cyst is carefully dissected from the ovarian tissue using blunt and sharp dissection.
Hydrodissection techniques help in minimizing trauma to the ovary.
3. Cyst Enucleation and Hemostasis
The cyst wall is gently separated from the ovarian cortex.
Hemostasis is ensured using bipolar coagulation, harmonic scalpel, or hemostatic agents.
The ovarian tissue is preserved as much as possible to maintain ovarian function.
4. Specimen Removal and Closure
The cyst is placed in a specimen retrieval bag and removed through a trocar site to prevent peritoneal contamination.
The ovary is reconstructed using fine sutures or hemostatic agents.
The peritoneal cavity is irrigated to remove any debris or blood.
Ports are closed, and skin incisions are sutured for optimal cosmetic results.
Advantages of Laparoscopic Ovarian Cystectomy
Compared to traditional open surgery, laparoscopy offers several benefits:
Minimally invasive approach with smaller incisions.
Reduced postoperative pain and faster recovery.
Lower risk of adhesion formation, improving future fertility.
Shorter hospital stay, often performed as an outpatient procedure.
Enhanced visualization, ensuring precise dissection and minimal damage to healthy ovarian tissue.
Early return to normal activities, usually within 7-10 days.
Potential Complications and Risk Factors
Although laparoscopic ovarian cystectomy is a safe and effective procedure, potential risks include:
Ovarian tissue damage, possibly affecting ovarian reserve.
Bleeding and hematoma formation, requiring hemostatic control.
Recurrence of cysts, particularly in PCOS and endometriosis.
Adhesion formation, though lower compared to open surgery.
Rare risk of malignant transformation, necessitating histopathological evaluation.
Recent Advancements in Laparoscopic Management of Ovarian Cysts
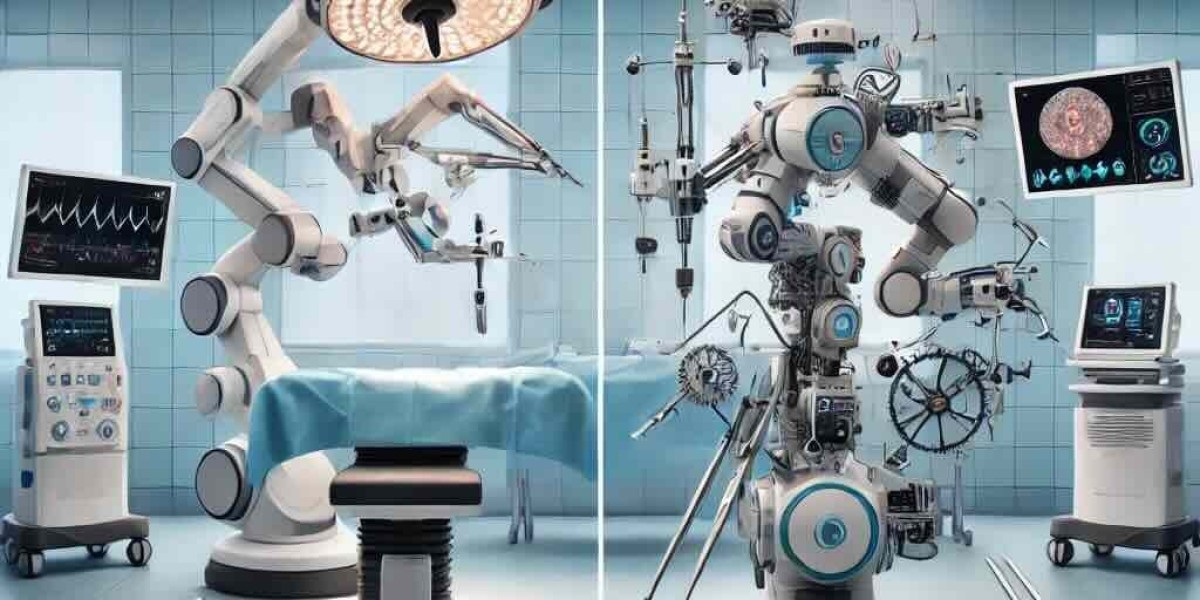
Robotic-Assisted Ovarian Surgery: Provides enhanced dexterity and precision, particularly for deep-seated or complex cysts.
Fluorescence-Guided Surgery: Helps in differentiating benign and malignant cysts intraoperatively.
Use of Hemostatic Sealants: Reduces blood loss and enhances ovarian healing.
Laser and Plasma Energy Devices: Allow tissue-selective dissection with minimal thermal damage.
Postoperative Care and Recovery
Most patients are discharged within 24 hours post-surgery.
Early ambulation is encouraged to prevent deep vein thrombosis (DVT).
A light diet is recommended initially, with a gradual return to normal eating.
Avoid strenuous activities and sexual intercourse for 4-6 weeks to allow proper healing.
Follow-up ultrasound may be recommended to assess ovarian function and ensure no recurrence.
Conclusion
Laparoscopy has revolutionized the management of ovarian cysts, offering a minimally invasive, safe, and effective alternative to open surgery. With advancements in robotic technology, energy devices, and surgical precision, the outcomes of laparoscopic ovarian cystectomy continue to improve, ensuring better recovery, reduced complications, and enhanced fertility preservation. For patients with symptomatic or complex ovarian cysts, laparoscopy remains the preferred surgical approach.
For the latest updates in minimally invasive gynecologic surgery, stay connected with the World Association of Laparoscopic Surgeons (WALS).