Laparoscopic surgery, a cornerstone of minimally invasive techniques, has transformed patient care by reducing recovery times and complications compared to open procedures. However, challenges like anatomical variability, obscured visibility in complex cases, and the risk of iatrogenic injuries (e.g., bile duct damage) persist. Enter Indocyanine Green (ICG), a fluorescent dye that, when paired with near-infrared (NIR) imaging, has emerged as a game-changer in laparoscopic surgery. Approved for clinical use since the 1950s, ICG’s role has expanded dramatically in recent decades, offering real-time visualization of critical structures and perfusion. This article explores how ICG enhances precision, safety, and outcomes in laparoscopic surgery, drawing from its applications across specialties like hepatobiliary, colorectal, and urologic procedures.
What is ICG and How Does It Work?
ICG is a water-soluble, tricarbocyanine dye injected intravenously or locally, depending on the procedure. It fluoresces bright green under NIR light (700–900 nm), a spectrum invisible to the naked eye but detectable by specialized laparoscopic cameras (e.g., Stryker 1588 AIM, PINPOINT). Cleared solely by the liver and excreted in bile, ICG is non-toxic with a wide safety margin, making it ideal for human use. In laparoscopy, NIR-equipped systems overlay this fluorescence onto the standard white-light view, providing surgeons with a dual-mode perspective—standard anatomy plus enhanced functional insights.
Key Applications in Laparoscopic Surgery
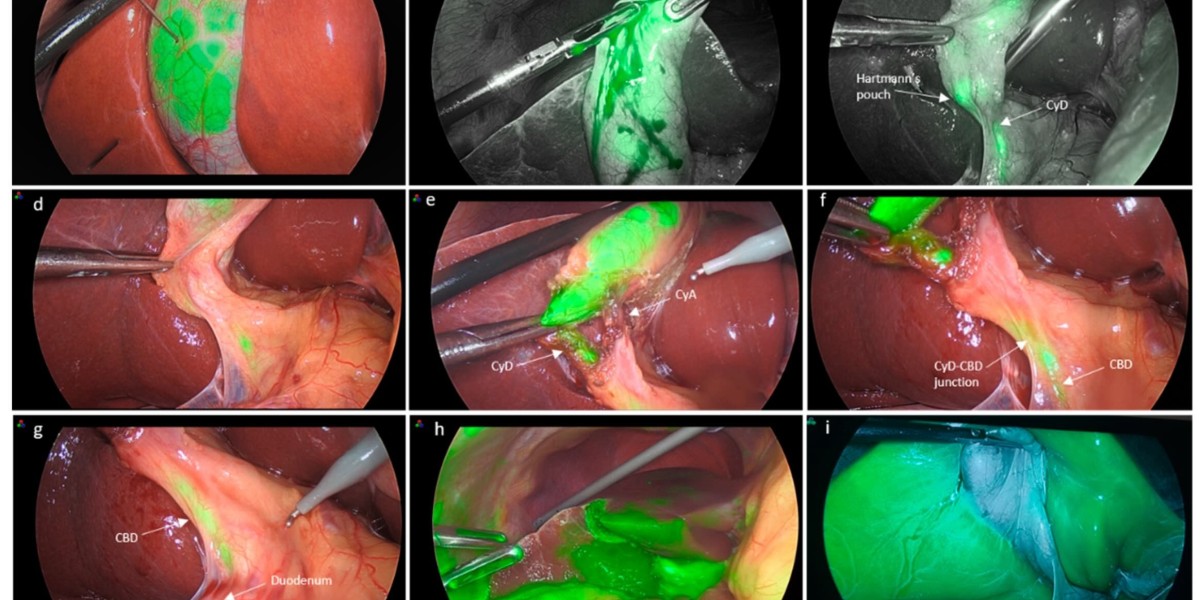
- Biliary Tree Visualization in Cholecystectomy
- Laparoscopic cholecystectomy (LC), the gold standard for gallbladder removal, carries a 0.3–0.8% risk of bile duct injury (BDI)—a dreaded complication. ICG fluorescence cholangiography addresses this by illuminating the cystic duct, common bile duct (CBD), and hepatic ducts in real time. Typically, 2.5 mg of ICG is injected intravenously 30 minutes to 6 hours before surgery, with optimal visualization achieved around 2–6 hours pre-incision. Studies suggest this reduces BDI risk compared to traditional radiographic cholangiography, offering a simpler, radiation-free alternative. For pediatric or acute cholecystitis cases, ICG’s clarity in inflamed or obese anatomies is a boon, as highlighted at WALS 2025 discussions.
- Perfusion Assessment in Colorectal Surgery
- Anastomotic leakage, occurring in 5–20% of colorectal resections, is a major concern linked to poor tissue perfusion. ICG fluorescence angiography allows surgeons to assess bowel vascularity intraoperatively. After injecting 5–7.5 mg of ICG IV post-resection, NIR imaging reveals perfusion at the anastomotic ends, guiding decisions on resection margins or protective stoma creation. Research shows a potential reduction in leak rates (e.g., 4% lower reoperation rates in some cohorts), though larger trials are needed. This was a focal point in Dr. Deep Goyal’s WALS 2025 talk on organ preservation in rectal cancer.
- Lymphatic Mapping and Tumor Localization
- In oncologic laparoscopy (e.g., colorectal, gastric, melanoma surgery), ICG aids sentinel lymph node (SLN) mapping. Injected peritumorally (0.5 mg/mL/kg with albumin), ICG highlights lymphatic drainage within 15–20 minutes, improving node harvest accuracy and staging. For right colectomies, it delineates nodal basins at the ileocolic vessels, refining lymphadenectomy—a debated aspect of minimally invasive techniques. This precision mirrors robotic surgery’s ethos, as seen with da Vinci systems at WALS 2025.
- Urologic and Vascular Applications
- In living-donor nephrectomies or ureteral surgeries, ICG (5 mg IV) assesses renal perfusion or ureteral course, reducing iatrogenic risks. In hernia repairs or vascular cases, it evaluates flap viability or amputation stump success, ensuring optimal healing—applications showcased in single-center series from India.
- Liver Resection and Anatomical Guidance
- Laparoscopic hepatectomy benefits from ICG’s dual staining methods: positive (portal vein injection for segment marking) and negative (systemic injection post-pedicle clamping for ischemic zones). Doses vary (e.g., 0.027–0.303 mg/100 mL), balancing fluorescence strength and clarity. This enhances anatomical resection precision, minimizing blood loss and complications.
Advantages of ICG in Laparoscopy
- Enhanced Safety: Real-time visualization reduces errors (e.g., BDI, vascular injury), aligning with safety principles like the Critical View of Safety in LC.
- Simplicity: No radiation or complex setup—ICG integrates into existing laparoscopic workflows.
- Versatility: From cholecystectomy to colorectal anastomosis, ICG adapts across specialties, as emphasized by WALS pioneers like Dr. R. K. Mishra.
- Cost-Effectiveness: Compared to intraoperative cholangiography or robotic add-ons, ICG is relatively affordable, though equipment costs (NIR systems) vary.
Limitations and Challenges
- Timing and Dosage: Optimal ICG administration varies—30 minutes suffices for biliary imaging, but lymphatic mapping needs precise timing. Overdosing can blur fluorescence, while underdosing weakens it.
- Equipment Dependency: Requires NIR-capable laparoscopes, not universal in all settings (e.g., rural India).
- Evidence Gaps: While promising (e.g., no BDI in some ICG-LC cohorts), statistical significance over standard methods isn’t fully established—larger randomized trials are pending.
- Learning Curve: Surgeons must interpret fluorescence alongside white light, a skill honed with experience.
ICG in Robotic Laparoscopy
The da Vinci Surgical System, a focus of your interest, integrates ICG via its Firefly fluorescence mode. A surgeon at the console uses master controls to toggle between standard and NIR views, guiding robotic arms with pinpoint accuracy. For instance, in prostatectomies or rectal resections, ICG highlights vascularity or tumor margins, enhancing the robot’s 3D precision. WALS 2025 showcased this synergy, with live demos underscoring ICG’s role in robotic cholecystectomy conversion rates dropping to near zero.
Future Directions
ICG’s trajectory in laparoscopy is bright. Artificial intelligence (AI) is being paired with ICG angiography to quantify perfusion (e.g., color maps in colorectal surgery), offering objective decision-making tools. Augmented reality could overlay ICG data onto anatomical models, further refining precision—a nod to futuristic labs you’ve explored. For Hindi-speaking regions like India, where laparoscopic adoption grows, ICG’s simplicity could democratize advanced care, as Dr. Mishra’s WALS efforts suggest.
Conclusion
Indocyanine Green has redefined laparoscopic surgery by illuminating what was once hidden—biliary anatomy, tissue perfusion, and lymphatic pathways. Its role in enhancing safety (e.g., reducing BDI in LC) and precision (e.g., guiding colorectal anastomoses) is undeniable, bridging traditional laparoscopy with robotic advancements. While challenges like standardization and equipment access remain, ICG’s integration into routine practice—evident at forums like WALS 2025—marks it as a standard-bearer for the future of minimally invasive surgery. For surgeons and patients alike, ICG isn’t just a dye; it’s a beacon of clarity in the operating room.