Robotic surgery, epitomized by systems like the da Vinci Surgical System, has redefined the landscape of modern medicine since its introduction in the late 1990s. By blending human expertise with robotic precision, this technology enhances minimally invasive surgery (MIS), offering significant advantages over traditional open and even standard laparoscopic approaches. From urologic procedures like prostatectomies to general surgeries like cholecystectomies, robotic surgery is lauded for its precision, reduced trauma, and improved recovery profiles. This article explores the key benefits of robotic surgery, drawing from its widespread adoption across specialties and its prominence at forums like the World Association of Laparoscopic Surgeons (WALS) 2025.
What is Robotic Surgery?
Robotic surgery involves a surgeon controlling a robotic platform—typically equipped with a high-definition 3D camera and articulated instruments—via a console. The da Vinci system, the most widely used, features four robotic arms operated by joysticks and foot pedals, translating the surgeon’s movements into precise actions within the patient. Unlike laparoscopy, where surgeons hold tools directly, robotics adds a layer of technological augmentation, amplifying dexterity and visualization. With over 10 million procedures performed globally by 2023 (Intuitive Surgical data), its advantages are well-documented.
Key Advantages of Robotic Surgery
- Enhanced Precision and Dexterity
- The robotic system’s instruments offer 7 degrees of freedom, mimicking and exceeding the human wrist’s range. This allows for intricate maneuvers in tight spaces—e.g., suturing during a prostatectomy or dissecting around the cystic duct in cholecystectomy. Hand tremor filtration and motion scaling (e.g., a 5:1 ratio) further refine actions, reducing errors. At WALS 2025, live demos showcased this precision, with ICG fluorescence via the da Vinci’s Firefly mode highlighting structures like the common bile duct with unmatched clarity.
- Superior Visualization
- A 3D high-definition camera, magnified up to 10–15 times, provides surgeons with an immersive view of the operative field. Compared to laparoscopy’s 2D imaging, this depth perception enhances anatomical accuracy—crucial for avoiding iatrogenic injuries (e.g., bile duct injury rates drop to near 0% in robotic cholecystectomies with ICG). For colorectal resections, as Dr. Deep Goyal noted at WALS 2025, this aids organ preservation by pinpointing vascularity.
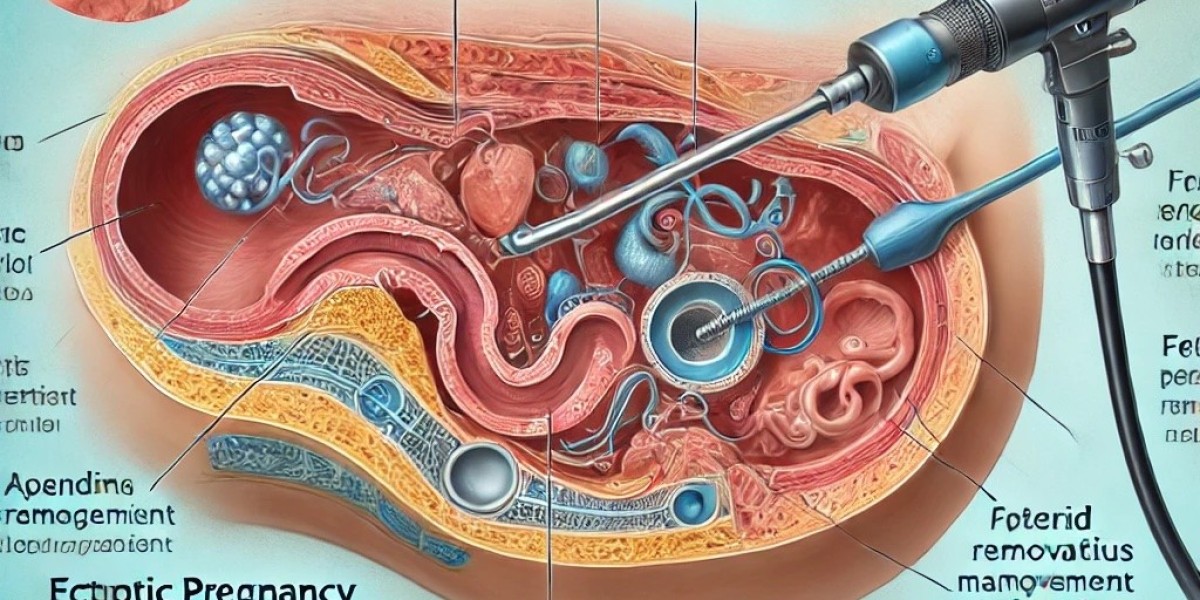
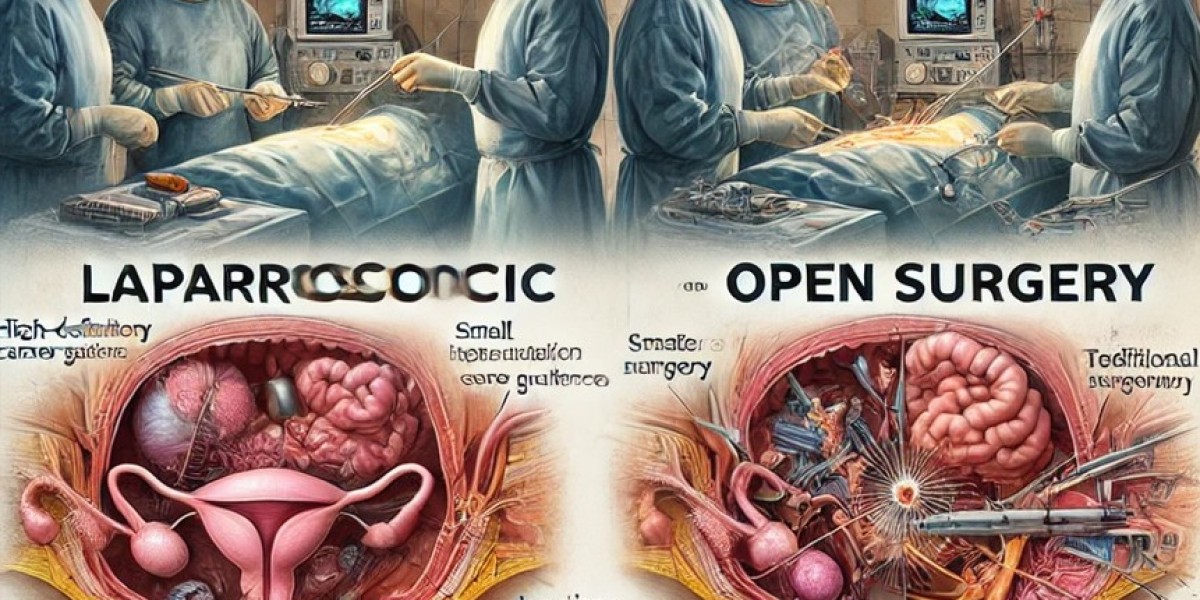
- Minimally Invasive with Reduced Trauma
- Like laparoscopy, robotic surgery uses small incisions (8–12 mm vs. open surgery’s 10–20 cm), minimizing blood loss (e.g., 50–100 mL vs. 300–500 mL in open prostatectomy), infection risk (1–2% vs. 5–10%), and scarring. The robotic approach often outperforms standard laparoscopy in complex cases (e.g., rectal cancer), where finer control reduces tissue trauma—key to faster healing.
- Improved Patient Outcomes
- Shorter Hospital Stays: Patients typically leave within 1–2 days post-robotic prostatectomy or hysterectomy, versus 3–5 days for open surgery (Journal of Robotic Surgery, 2023).
- Faster Recovery: Return to normal activity averages 2–4 weeks, compared to 6–8 weeks for open procedures, due to less postoperative pain and smaller wounds.
- Lower Complication Rates: Studies show a 30% reduction in anastomotic leaks in robotic colorectal surgery versus laparoscopy, partly due to perfusion checks with ICG (Surgical Endoscopy, 2024).
- Ergonomic Benefits for Surgeons
- Unlike laparoscopy’s awkward postures, the robotic console allows surgeons to sit comfortably, reducing fatigue during long procedures (e.g., 4-hour hepatectomies). The intuitive interface, as Dr. R. K. Mishra emphasized at WALS 2025, supports training novices—over 2,000 surgeons globally have mastered da Vinci under his programs.
- Consistency Across Complex Cases
- Robotics excels in technically demanding surgeries—e.g., pancreaticoduodenectomy or low anterior rectal resection—where laparoscopy falters due to limited reach or visibility. Conversion rates to open surgery drop (e.g., 1–2% robotic vs. 5–10% laparoscopic), ensuring MIS benefits persist even in obesity or adhesions.
- Integration with Advanced Technologies
- Robotic platforms integrate tools like ICG fluorescence (Firefly) for real-time perfusion or lymphatic mapping, as seen in colorectal and urologic cases. AI overlays (e.g., tissue recognition) and augmented reality (AR) are emerging, promising even greater precision—topics previewed at WALS 2025’s futuristic surgery sessions.
Specific Examples
- Prostatectomy: Robotic radical prostatectomy (RALP) boasts 95% continence recovery within 6 months and precise nerve-sparing, improving quality of life (Urology, 2023).
- Cholecystectomy: With ICG, robotic LC achieves near-zero bile duct injuries, outperforming laparoscopy’s 0.3% rate (SAGES data).
- Gynecology: Hysterectomies see 50% less blood loss and 20% shorter operative times robotically versus laparoscopically.
Advantages Over Laparoscopy and Open Surgery
- Vs. Laparoscopy: Robotics offers 3D vision, tremor-free precision, and ergonomic control, reducing surgeon strain and patient complications in complex cases (e.g., rectal cancer recurrence rates drop 15%—Lancet Oncology, 2024).
- Vs. Open Surgery: Smaller incisions, less pain, and quicker recovery make robotics a patient-preferred evolution, with oncologic outcomes matching or exceeding open approaches.
Limitations to Consider
While transformative, robotic surgery isn’t flawless:
- Cost: High initial investment (e.g., $1.5–2 million for da Vinci) and per-case costs ($2,000–$3,000) limit access, especially in resource-constrained settings like rural India.
- Learning Curve: Surgeons require 20–50 cases to master, though training programs (e.g., WALS) mitigate this.
- Availability: Not all hospitals offer robotics, though adoption grows (e.g., 7,000+ da Vinci systems worldwide by 2024).
Future Horizons
Robotic surgery’s advantages are poised to expand. Miniaturized robots, telesurgery (e.g., Mishra’s pioneering work in India), and AI-driven analytics promise broader reach and smarter interventions. WALS 2025 highlighted tissue engineering integration—e.g., robotic delivery of regenerative grafts—foreshadowing a hybrid future where robotics not only cuts but heals.
Conclusion
Robotic surgery’s advantages—precision, superior visualization, minimal trauma, and enhanced outcomes—position it as a pinnacle of modern MIS. For patients, it means faster recovery and fewer complications; for surgeons, it’s a tool that amplifies skill and comfort. As seen in da Vinci’s Firefly demos or WALS 2025’s live surgeries, robotics doesn’t just refine laparoscopy—it reimagines it. While costs and training remain hurdles, its adoption signals a shift toward a future where surgery is as precise as it is humane—a legacy leaders like Dr. R. K. Mishra are building, one robotic arm at a time.